Your Game: Pain Free Living
Dedicated to helping patients live life fully, Orthopedic Associates physicians are recognized as leaders in their field, thanks to their clinical expertise and dedication to patient care.
Understanding That Pain in Your Knee
And how to address the most common problems for tennis players
Story by Andrew Parker, MD
This story appeared in the Spring 2018 issue of Colorado Tennis.
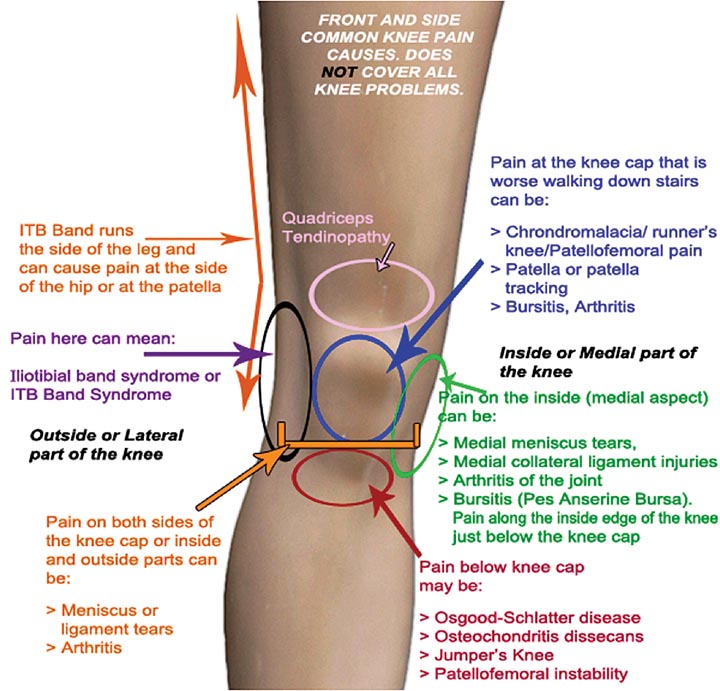
In the last issue, Dr Brian Larkin discussed knee pain related to degenerative arthritis and the different types of injections, from cortisone to biologics that could prolong time on the court. In this installment, we will discuss the non-arthritic causes of knee pain that may affect your performance on the court, the causes, and some treatment options. Like everything in medicine there is some overlap though, and often a simple diagnosis of a meniscus tear masks a bigger picture of degenerative arthritis. The two general categories that we will cover today are overuse injuries and mechanical conditions.
Overuse injuries are one of the more common presenting problems that we see regarding overhead sports. Sometimes seen in the high school athlete preparing for an upcoming season, these issues are most commonly seen in the “weekend warrior”, and include a variety of tendonitis and inflammatory problems from patellar tendonitis, IT band tendonitis, and chondromalacia, or mild kneecap arthritis.
Tendonitis refers to irritation or inflammation of the soft tissue that connects the bones around the knee. Hence, patellar tendonitis is inflammation of the tendon that connects the kneecap to the shin bone.
Tendons, like other soft tissue, respond positively and negatively to activity and lack of activity. Most tendonitis issues in tennis start with the common story of a period of inactivity (winter) followed by a sudden ramp-up in activity that involves excessive strain (stretch) of tissue that overwhelms the tissue’s ability to tolerate the load or flexibility that the activity demands. Fortunately, these are all issues that have a solution; unfortunately, they may involve time and additional effort. Specifically, most of these problems can be avoided or addressed with activity modification (a slow return to sport) complimented with a gradual and progressively increasing physical challenge. The most important adjunct to this is a good and consistent stretching program.
Chondromalacia, or mild kneecap arthritis, is also a type of overuse injury. As the surface cartilage on the back of the kneecap begins to age, it creates mechanical irritation with quadricep dominate sports (tennis), and an inflammatory reaction ensues. As with other overuse injuries, a gradual progression back to sports, combined with progressive, pain-free challenge, and most importantly a good flexibility program minimize these issues during the Spring ramp-up and throughout the season.
Mechanical conditions are usually the result of injury. As we age, the significance of the injury may decrease, and there may be more of a degenerative (arthritis) component. The most common of these conditions are meniscal tears. The menisci (one inside-medial and one outside-lateral) are the cushioning cartilage gaskets that support the joint surface cartilage (which wears out with arthritis). These gaskets move with the knee, and with pivoting sports, are at risk for damage. Unfortunately, they have poor blood supply which is what puts them at risk and eliminates the potential for healing. Patients usually present with a minor episode, and activity related aching and swelling. Rest may improve the symptoms, but persistent issues are best dealt with through a minor outpatient “scope”. Fortunately, major ligament injuries, like ACL tears, are rare in tennis, but may require surgery for a full return to sport.
Injection Inspection
Can injections help keep you on the court and out of pain?
Story by Brian Larkin, MD
This story appeared in the Spring 2018 issue of Colorado Tennis.

Nowadays, you cannot turn on the TV, open the newspaper, or surf the web without being bombarded with all sorts of options for injections in painful, arthritic knees. Many options promise quick pain relief and improved function. Below is a brief summary of the options that exist.
Steroid injections. Steroid (cortisone) injections target the inflammation present due to knee arthritis. These are commonly combined with local anesthetic and provide predictable pain relief. Patients can get these about every 3-4 months as needed. There is a possibility that multiple injections into a single joint may lead to degradation of the tissues present there.
Viscosupplementation injections. Viscosupplementation injections are composed of hyaluronic acid. Hyaluronic acid is a component of synovial fluid, the cushioning liquid in the knee. These medications are derived from the comb of a rooster. Trade names include Synvisc, Orthovisc, Gel One, Euflexxa, Monovisc, and many others. Insurance providers may approve these injections every 6 months. In the setting of advanced arthritis, certain patients do not get much relief with these shots.
Platelet-Rich Plasma (PRP). Platelet-rich plasma is a portion of a patient’s own blood. Blood is drawn out of the patient’s vein and then spun down to concentrate the platelets and growth factors. This concentrated solution is then injected back into the knee joint. Professional athletes have sought these types of injections with the goal of decreasing inflammation and enhancing the healing process. PRP injections are not currently covered by most insurance plans.
Stem cell injections. Stem cell injections have been gaining more excitement in the lay press about the potential to reverse arthritis. Unfortunately, there are no strong studies that support the idea that stem cell injections into the knee can regrow cartilage and reverse arthritis. Some are able to get relief from the injections due to an anti-inflammation effect. There are a number of sources where the stem cells can be harvested and multiple different preparations that exist. It is important to ask your provider about these details. Similar to PRP injections, these are not currently covered by most insurance plans.
As you can see, there are a number of options that exist. In order to tailor the treatment of any patient’s knee arthritis, a detailed discussion with your orthopedic surgeon that covers your symptoms, x-ray findings, and goals of treatment should be had on a regular basis. The goal is to minimize your symptoms and keep you on the court playing at your top capacity.
Through our shared partnership between Orthopedic Associates and USTA Colorado, we are committed to educating our patients about all of these options and tailoring each patient’s specific treatment plan.